Love, Lust, and Relapse in Early Recovery
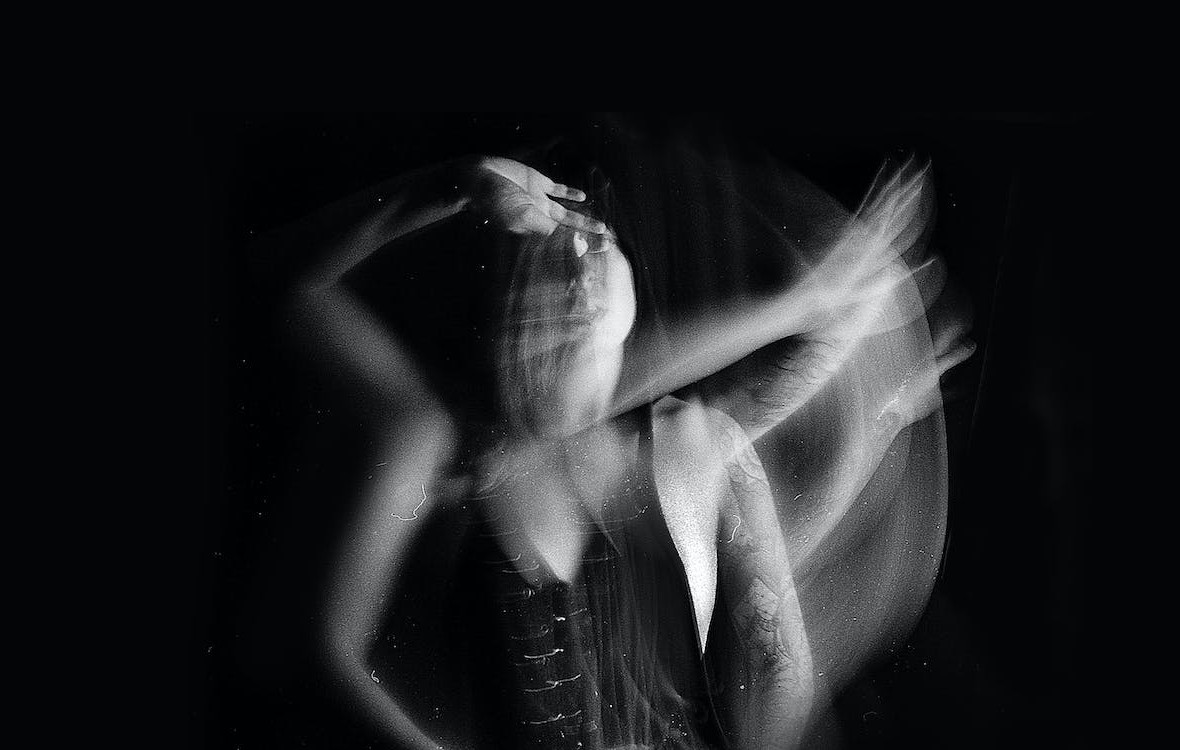
In early recovery, life feels raw, stripped of the chemical fog that once dulled everything. The world suddenly comes back in colour. You start to feel again, laugh again, want again. And in that wave of returning emotion, love can look like the next high.
It’s the oldest trap in recovery, falling into a new relationship too soon. On the surface, it feels like progress, connection, passion, hope. But underneath, it’s often the same old addiction wearing a prettier face. Because when you’ve spent years using substances to feel good, the rush of new romance hits the same brain receptors. The dopamine doesn’t care if it comes from a bottle or a body.
The Substitute High
Addiction is about escape. Drugs, alcohol, gambling, sex, they all serve the same purpose, to avoid pain, silence fear, and feel alive. When substances disappear, the brain scrambles to find something else to fill the void. Love and lust fit perfectly. The chemistry of new love is intoxicating. Dopamine spikes, serotonin floods, and suddenly, recovery feels easy again. You’re alive, confident, glowing. You tell yourself you’ve moved on from your old life, but what’s really happening is substitution. The person becomes the drug.
This “relationship high” often happens before emotional stability returns. Early recovery is still about rebuilding trust, learning boundaries, and managing triggers. But addiction rewires the reward system, making intensity feel like connection. The result? Codependent relationships that burn hot and crash hard.
Why Rehab Rules Forbid Romance
Most rehab programmes have an unwritten rule, no relationships in the first year of recovery. Not because love is bad, but because it’s too powerful. Early recovery is like emotional infancy, everything feels new, fragile, and overwhelming. You’re learning to sit with loneliness, fear, and boredom without numbing. You’re relearning identity after years of chaos. Add romance to that equation, and the emotional turbulence doubles. Suddenly, your mood depends on another person. A fight feels like a relapse trigger. A breakup can send you straight back to your old coping mechanism.
It’s not that relationships are impossible, they’re just risky when your emotional foundation isn’t stable yet. Recovery asks you to build self-worth from the inside out, not through another person’s validation.
The “Saviour Syndrome”
In recovery spaces, relationships often form between people with shared trauma. There’s an unspoken bond, a sense that “you get me.” You see someone who understands your pain, your shame, your cravings. It feels real, deep, fated. But it’s also dangerous. Two people in early recovery are like two survivors clinging to each other in a storm. They mistake shared pain for compatibility. What starts as mutual healing quickly becomes mutual dependency. Instead of focusing on personal growth, each becomes the other’s project.
One plays the rescuer, the other the rescued. Both roles feed ego and fear. And when one person slips, emotionally or chemically, the other usually follows. In recovery, love without boundaries isn’t connection. It’s collapse.
The Dopamine Rollercoaster
Every addict understands dopamine, that chemical hit that makes you feel invincible one moment and worthless the next. Love runs on the same circuitry. The highs are euphoric; the lows are unbearable. That’s why relationships in early recovery often mirror the cycle of addiction itself. You chase intensity instead of intimacy, passion instead of peace. Arguments feel like withdrawal, reconciliation feels like a fix. You start timing your emotional state around another person instead of your recovery routine.
When that person leaves, or even just pulls away, the emptiness feels familiar. And so, many relapse. Not because they want the substance, but because they can’t face the pain of loss without it.
Lust, Loneliness, and the Body’s Betrayal
Sobriety doesn’t switch off desire. In fact, it often reignites it. After months or years of numbing, your senses wake up, and so does your libido. But physical intimacy in early recovery carries emotional weight the body doesn’t yet know how to handle. Lust becomes another distraction, another escape. It’s easy to confuse attraction with affection, validation with love. You mistake chemistry for connection, forgetting that addiction isn’t picky about its outlet. Whether it’s sex, substances, or status, the pattern is the same: seek the rush, avoid the void.
This doesn’t mean sex is bad, it means it’s loaded. In early recovery, every craving, impulse, and emotional high deserves scrutiny. The body might be sober, but the brain is still negotiating its relationship with pleasure.
The Mirror Effect
Dating in early recovery often exposes the very wounds that led to addiction. Insecure attachment, fear of abandonment, low self-worth, all of it comes rushing back when you start to care for someone. The difference is, there’s nowhere to hide now. No drink to numb rejection, no drug to drown insecurity.
Your partner becomes a mirror reflecting back every unresolved issue you carry. The temptation is to run, or relapse. But if handled carefully, that mirror can also be a teacher. Healthy relationships require emotional honesty, patience, and vulnerability, all the same qualities recovery demands. The challenge is not to use love as a distraction, but as a reflection.
Why Loneliness Feels Like Withdrawal
One of the hardest parts of early recovery is the loneliness. Without the social circles of using, without the chemical comfort of substances, silence feels unbearable. That’s why new relationships feel like salvation. They make the loneliness vanish, temporarily.
But loneliness isn’t a symptom to fix, it’s a signal to understand. It’s your body telling you that connection matters, but that it must start with yourself. Jumping into a relationship before learning self-companionship is like skipping physical therapy after surgery, you might walk faster, but you’ll walk crooked. Recovery teaches you to sit in the discomfort of solitude until it stops feeling like punishment. Only then can connection become a choice, not a crutch.
The Relapse Nobody Talks About
Romantic relapse happens quietly. It starts with neglecting meetings, skipping therapy, or compromising boundaries. “I don’t need to go tonight, we’re having dinner.” “They don’t like me sharing about us in group.” Slowly, recovery takes the back seat. Then, when the relationship collapses, as many early ones do, the emotional fallout feels unbearable. The addict brain, wired for relief, starts whispering, just one drink, one hit, one escape. And that’s how heartbreak becomes a relapse trigger.
In truth, many people relapse not because of old habits, but because of new heartbreak. The pain of losing love feels worse than detox. It’s a reminder that addiction was never really about the drug, it was about trying not to feel.
The Self-Love Myth
“Focus on self-love first” is good advice, but it’s also vague. What does self-love actually mean in recovery? It’s not bubble baths or affirmations, it’s boundaries. It’s learning to say no to chaos, including romantic chaos. It’s showing yourself the same consistency you once reserved for substances or partners.
Self-love in recovery means treating your peace as non-negotiable. It means realising that someone else’s attention is not proof of your worth. It means being able to be alone without falling apart. Until that foundation is built, every relationship will shake it loose.
The Healthy Kind of Love
Not all relationships in recovery are doomed. Some become powerful support systems, but only when both people are grounded in their own growth. Healthy love in recovery isn’t about saving or fixing each other. It’s about walking side by side. It’s about honesty, accountability, and patience. It’s about celebrating progress without becoming the purpose.
Love can heal, but only if it’s built on truth, not trauma. The difference between a relapse trigger and a recovery partner is simple, one helps you escape yourself, the other helps you face yourself.
Red Flags in Early Recovery Dating
- Intensity disguised as intimacy. If it feels too good too soon, it’s probably a high, not a bond.
- Neglecting recovery routines. If you’re skipping meetings or therapy to be with someone, the warning light’s on.
- Emotional volatility. If arguments feel like withdrawals or make you crave, you’re in dangerous territory.
- Validation dependence. If your mood depends on their texts, you’ve replaced one addiction with another.
- Isolation. If you’ve pulled away from your support system, the relationship isn’t love, it’s relapse waiting to happen.
Awareness doesn’t mean avoidance, it means you choose connection consciously, not compulsively.
Love as a Mirror for Growth
Eventually, love in recovery becomes possible, and profound. When it’s no longer a substitute for addiction, it becomes a mirror for growth. You learn vulnerability without collapse, commitment without control, and intimacy without intoxication. The right relationship won’t replace recovery, it will deepen it. It will teach you the difference between connection and consumption, between companionship and dependency.
Love, when met with sobriety, stops being the next high and becomes the next lesson.